Headaches
Author: Jerry Song
Headaches are one of the most common neurological complaints encountered in clinical practice, affecting individuals across various demographic groups. They can be broadly categorised into primary and secondary headaches, with each category encompassing multiple subtypes. Understanding the etiology of these headaches and the demographics most likely to suffer from them is crucial for effective diagnosis and management.

- Primary Headaches
Primary headaches are not caused by an underlying medical condition but are disorders themselves. The main types include migraines, tension-type headaches (TTH), and cluster headaches.
- Migraine
Migraine is a recurrent headache disorder characterised by moderate to severe pain, typically unilateral and pulsating in nature. The pain is often accompanied by nausea, vomiting, and sensitivity to light and sound. Migraines can be preceded by aura, which includes visual disturbances or other neurological symptoms.
Etiology: The exact cause of migraines is not fully understood, but it is believed to involve a combination of genetic, environmental, and neurological factors. There is evidence suggesting abnormal brain activity and blood flow changes, as well as dysfunction in the trigeminovascular system.
Demographics: Migraines affect approximately 12% of the global population, with a higher prevalence in women than men (about 3:1 ratio). They are most common in individuals aged 18 to 44, particularly among women of childbearing age due to hormonal fluctuations. There is also a genetic predisposition, as migraines tend to run in families.
- Tension-Type Headache (TTH)
Tension-type headaches are the most common type of primary headache. They are characterised by bilateral, mild to moderate pain, often described as a tight band around the head. These headaches can last from 30 minutes to several days.
Etiology: The etiology of TTH is believed to involve muscle tension and stress. Psychological factors such as anxiety and depression are also associated with TTH. The pain is thought to result from peripheral activation or sensitisation of myofascial nociceptors.
Demographics: Tension-type headaches affect up to 80% of the population at some point in their lives. They are slightly more common in women than men and are most frequently reported by individuals in their 30s and 40s. Stressful life situations and poor posture are common triggers.
- Cluster Headache
Cluster headaches are characterised by severe, unilateral pain, typically around the eye or temple, often accompanied by autonomic symptoms such as tearing, nasal congestion, or eyelid swelling. These headaches occur in clusters, with multiple attacks over weeks or months, followed by periods of remission.
Etiology: The exact cause of cluster headaches is unknown, but they are thought to involve abnormalities in the hypothalamus, leading to dysregulation of circadian rhythms. Genetic factors may also play a role, though they are less prominent than in migraines.
Demographics: Cluster headaches are rare, affecting about 0.1% of the population. They are more common in men than women (about 4:1 ratio) and typically begin between the ages of 20 and 40. Smoking and alcohol consumption are significant risk factors.
- Secondary Headaches
Secondary headaches are symptomatic of an underlying medical condition. The pain is often due to infection, trauma, vascular disorders, or other systemic issues. Common types include:
- Medication Overuse Headache (MOH)
Medication overuse headache, also known as rebound headache, occurs as a result of frequent use of headache medications. The headache is usually present upon waking and can resemble a tension-type headache or migraine.
Etiology: MOH is caused by the regular use of analgesics or triptans for headache relief, leading to a cycle of overuse and increased headache frequency.
Demographics: MOH is more prevalent in women, particularly those aged 30 to 50. It is also common among individuals with a history of chronic headaches, such as migraines or tension-type headaches.
- Sinus Headache
Sinus headaches are caused by inflammation or infection of the sinuses, leading to pressure and pain in the forehead, cheeks, and eyes. These headaches are often associated with sinusitis and may be accompanied by nasal congestion, fever, and facial swelling.
Etiology: Sinus headaches occur due to inflammation of the sinus cavities, often secondary to infection (viral or bacterial) or allergic reactions. The pain results from increased pressure within the sinuses.
Demographics: Sinus headaches are more common in individuals with a history of allergies or chronic sinusitis. They are equally prevalent among men and women and can affect all age groups, though they are more common in adults.
- Cervicogenic Headache
Cervicogenic headache is a secondary headache caused by disorders of the cervical spine and its components, such as intervertebral discs, facet joints, or cervical muscles. The pain is typically unilateral and may radiate from the neck to the front of the head.
Etiology: Cervicogenic headaches result from cervical spine disorders, such as osteoarthritis, herniated discs, or whiplash injuries. The pain is believed to originate from the convergence of nociceptive input from the cervical spine and trigeminal nerve.
Demographics: This type of headache is more common in individuals with neck trauma or chronic neck pain, particularly those aged 30 to 50. It is slightly more prevalent in women than men.
If you or someone you know are dealing with headaches, musculoskeletal pain, or even myofascial trigger points, book in an appointment to see Jerry now for an initial consultation so we can assess your condition and come up with an appropriate and tailored treatment plan to manage your pain. Simply click this booking link for the myotherapy initial consultation with our experienced myotherapists.
















 The pathophysiology of CTS is complex and involves mechanical compression, ischemia, and inflammation of the median nerve within the carpal tunnel. Predisposing factors such as wrist anatomy, repetitive hand movements, trauma, hormonal changes, and systemic diseases contribute to the development of CTS. Compression of the median nerve leads to impaired nerve conduction, demyelination, and axonal degeneration, resulting in sensory and motor deficits in the affected hand.
The pathophysiology of CTS is complex and involves mechanical compression, ischemia, and inflammation of the median nerve within the carpal tunnel. Predisposing factors such as wrist anatomy, repetitive hand movements, trauma, hormonal changes, and systemic diseases contribute to the development of CTS. Compression of the median nerve leads to impaired nerve conduction, demyelination, and axonal degeneration, resulting in sensory and motor deficits in the affected hand. If you or someone you know are dealing with CTS, musculoskeletal pain, or even myofascial trigger points, book in an appointment to see us now for an initial consultation so we can assess your condition and come up with an appropriate and tailored treatment plan to manage your pain.
If you or someone you know are dealing with CTS, musculoskeletal pain, or even myofascial trigger points, book in an appointment to see us now for an initial consultation so we can assess your condition and come up with an appropriate and tailored treatment plan to manage your pain.

 Individuals with LCS often experience chronic low back pain, hip pain, and tightness in the hip flexors. Dysfunction in the lumbar-pelvic region may contribute to secondary symptoms such as sacroiliac joint dysfunction and hip joint impingement. Additionally, LCS can impair functional movement patterns, affecting activities such as walking, standing, and squatting. Reduced hip mobility and stability may also predispose individuals to compensatory movements and increased risk of injury during physical activities.
Individuals with LCS often experience chronic low back pain, hip pain, and tightness in the hip flexors. Dysfunction in the lumbar-pelvic region may contribute to secondary symptoms such as sacroiliac joint dysfunction and hip joint impingement. Additionally, LCS can impair functional movement patterns, affecting activities such as walking, standing, and squatting. Reduced hip mobility and stability may also predispose individuals to compensatory movements and increased risk of injury during physical activities.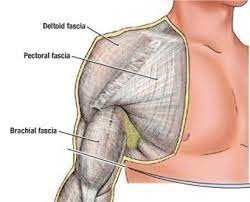 Some of the common fascial conditions include Myofascial Pain Syndrome (MPS), which is a pathology characterised by the development of trigger points within fascial tissues. These trigger points can lead to localised or referred pain, muscle stiffness, and reduced range of motion. Another fascial condition that may arise is fascial adhesions, which occur when collagen fibers in the fascial matrix become distorted or adhered, resulting in restricted movement and impaired tissue glide. This can contribute to chronic pain and dysfunction.
Some of the common fascial conditions include Myofascial Pain Syndrome (MPS), which is a pathology characterised by the development of trigger points within fascial tissues. These trigger points can lead to localised or referred pain, muscle stiffness, and reduced range of motion. Another fascial condition that may arise is fascial adhesions, which occur when collagen fibers in the fascial matrix become distorted or adhered, resulting in restricted movement and impaired tissue glide. This can contribute to chronic pain and dysfunction.



