The Melbourne Marathon is one of the most prestigious running events in Australia, drawing thousands of participants each year. Whether you’re an elite runner aiming for a personal best or a weekend warrior finishing your first marathon, crossing the finish line is a huge achievement. However, after the exhilaration of completing the race fades, your body may be feeling the effects of the physical toll. This is where Myotherapy and Remedial Massage come into play as crucial tools for post-race recovery.
Running 42.2 kilometers (or even the shorter events) places significant stress on the muscles, joints, and connective tissues. Recovery is essential not just for relieving pain and discomfort but also for ensuring long-term mobility and preventing injury. This article will discuss how Myotherapy and Remedial Massage can assist in post-race recovery and why every runner should consider incorporating these therapies into their recovery plan.
Understanding the Impact of a Marathon on the Body
Completing a marathon puts immense strain on the body, particularly the lower limbs. During a race, runners are at risk of the following:
- Muscle fatigue: Prolonged running leads to muscle fatigue, particularly in the legs, hips, and core. The repetitive impact can cause microtears in muscle fibers, leading to post-race soreness, commonly known as delayed onset muscle soreness (DOMS).
- Joint stress: The knee, hip, and ankle joints endure repeated pounding over the course of the marathon, which can cause inflammation, stiffness, and pain.
- Tightness and muscle imbalances: After a long-distance race, muscles such as the hamstrings, quadriceps, and calves may become tight, leading to imbalances that can cause discomfort or increase the risk of injury.
- Reduced flexibility and mobility: Long runs can lead to stiffness, affecting range of motion in key areas like the hips, knees, and ankles.
Given these physical demands, the post-race recovery process is critical in helping the body heal and preventing longer-term issues. This is where Myotherapy and Remedial Massage can play an essential role.
What Is Myotherapy and Remedial Massage?
Myotherapy is a specialised form of manual therapy that focuses on the assessment, treatment, and rehabilitation of musculoskeletal pain and dysfunction. It combines deep tissue massage, trigger point therapy, and muscle stretching with other advanced techniques such as dry needling, myofascial cupping, joint mobilisation, and corrective exercises.
Remedial massage focuses on relieving muscle tension and addressing muscular imbalances caused by overuse, injury, or poor posture. It involves targeted, deep-tissue massage techniques that can help alleviate pain, improve mobility, and accelerate recovery. Both therapies are highly effective in addressing post-race muscle fatigue, soreness, and stiffness.
How Myotherapy and Remedial Massage Aid Post-Marathon Recovery
1. Reducing Muscle Soreness (DOMS)
Delayed onset muscle soreness (DOMS) is a common post-marathon complaint that usually sets in 24 to 48 hours after the race. Myotherapy and remedial massage can help reduce the severity of DOMS by increasing blood flow to the affected areas, promoting the removal of metabolic waste products such as lactic acid, and providing the necessary nutrients for tissue repair.
By reducing inflammation and alleviating the muscle tightness that contributes to DOMS, runners can experience less post-race discomfort and recover more quickly.
2. Promoting Faster Healing and Tissue Repair
Myotherapy and remedial massage stimulate circulation, which increases the supply of oxygen and nutrients to damaged muscles. This enhanced blood flow promotes tissue repair and accelerates the healing process, reducing the amount of time it takes for sore muscles to recover after a race.
Myotherapy, in particular, can target deeper layers of muscle and connective tissue, releasing adhesions or “knots” that may have developed during the run. By releasing these restrictions, runners can avoid the development of chronic muscular tension.
3. Improving Joint Mobility and Flexibility
Stiffness in the joints, particularly in the knees, hips, and ankles, is common after a marathon due to the repetitive impact of running. Myotherapy and remedial massage work to restore mobility in these joints by addressing muscle imbalances, tightness, and restrictions in the surrounding tissues. Gentle joint mobilisation techniques used in myotherapy can further enhance range of motion, making it easier to move freely and reducing the risk of post-race injuries.
By restoring normal muscle function and range of motion, these therapies help prevent compensatory movement patterns that could lead to further strain or injury.
4. Relieving Muscle Tightness and Imbalances
After running for extended periods, certain muscles may become tight or overworked, while others become weakened or underutilised. This imbalance can lead to altered movement patterns and increase the risk of injury. Myotherapy and remedial massage target these imbalances by releasing tight muscles and strengthening weaker areas.
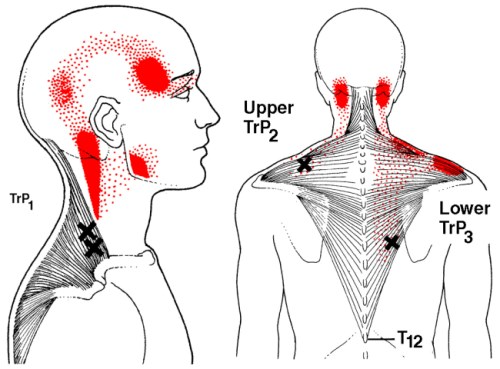
Trigger point therapy, a technique often used in both myotherapy and remedial massage, targets specific areas of muscle tension or “knots” that can cause referred pain. Releasing these trigger points can relieve tightness and restore balance to the musculoskeletal system.
5. Preventing Injury and Supporting Long-Term Recovery
Recovery is not just about feeling better in the short term; it’s also about preventing future injuries. Muscles and joints that have been subjected to the repetitive impact of a marathon are at risk of injury if they are not properly cared for during the recovery phase.
Myotherapy and remedial massage can help identify and address areas of potential weakness or imbalance that may lead to injuries such as tendinitis, IT band syndrome, or plantar fasciitis. By addressing these issues early, athletes can avoid downtime and continue training more effectively.
Key Techniques Used in Myotherapy and Remedial Massage for Runners
Both myotherapy and remedial massage incorporate various techniques to aid in post-race recovery. Some of the key methods include:
- Deep Tissue Massage: Focuses on releasing deep muscle tension and breaking down adhesions, allowing for better muscle function and mobility.
- Trigger Point Therapy: Targets specific points of tension in the muscles that can cause referred pain and tightness, releasing them to restore muscle balance.
- Dry Needling: A technique used in myotherapy to release tight muscle bands and reduce pain by inserting fine needles into specific trigger points. This helps reduce inflammation and promote muscle relaxation.
- Myofascial cupping: Myofascial cupping involves the use of suction cups to create negative pressure on the skin, lifting and separating the underlying tissues. Loosening tight fascia and muscle adhesions can restore normal tissue mobility and reduce pain.
- Myofascial Release: Helps to release tension in the connective tissue (fascia) surrounding the muscles, reducing stiffness and improving mobility.
-
Joint Mobilisation: Gently moves joints through their natural range of motion to restore mobility, especially in the hips, knees,
and ankles.

When to Get Myotherapy or Remedial Massage Post-Marathon
The timing of post-race treatment is essential for effective recovery. It is generally recommended to wait at least 24–48 hours after the marathon before undergoing deep tissue or intensive massage therapy to allow the initial inflammation and swelling to subside. Light recovery massages can be beneficial immediately after the race to improve circulation and relax the muscles. After a few days, deeper tissue work and myotherapy can be highly effective in addressing muscle tightness, imbalances, and soreness.
If you or someone you know are dealing with post-race soreness and tightness, musculoskeletal pain, or even myofascial trigger points, book an appointment to see Jerry now for an initial consultation so we can assess your condition and come up with an appropriate and tailored treatment plan to manage your pain. Simply click this
booking link for the myotherapy initial consultation with our experienced
myotherapists.









 .
. 





















