Repetitive strain injury (RSI)
Repetitive strain injury (RSI)
Repetitive strain injury (RSI) refers to a spectrum of conditions caused by repetitive movements and overuse of particular body parts, often leading to pain, discomfort, and functional impairment. RSIs are common in occupations and activities involving repetitive motions, prolonged exertion, or maintaining awkward positions.

RSI manifests in several forms, each affecting different anatomical structures:
- Carpal Tunnel Syndrome (CTS): Compression of the median nerve within the carpal tunnel of the wrist, leading to numbness tingling, and weakness in the hand.
- Tendinitis: Inflammation of tendons, commonly affecting the shoulders, elbows, and wrists. Examples include tennis elbow (lateral epicondylitis) and golfer’s elbow (medial epicondylitis)
- Bursitis: Inflammation of the bursae, small fluid-filled sacs that cushion bones and tendons, typically occurring in the shoulder, elbow and hip.
- De Quervain’s Tenosynovitis: Inflammation of the sheath surrounding the thumb tendons, causing pain and swelling at the base of the thumb.
- Thoracic Outlet Syndrome (TOS): Compression of nerves or blood vessels between the collarbone and first rib, causing pain in the neck, shoulders, and arms.
The primary causes of RSI include:
- Repetitive Movements: Continuous, repetitive actions such as typing, using a mouse, or assembly line work.
- Forceful Exertions: Activities requiring significant physical effort, including lifting heavy objects or using tools.
- Sustained Postures: Maintaining fixed positions for extended periods, such as sitting at a desk or standing without adequate breaks.
- Poor Ergonomics: Inadequate workstation setup, improper body mechanics, and poor posture.

Demographic Analysis:
RSI predominantly affects adults aged 25-50, particularly those in occupations involving repetitive tasks or prolonged static positions. Office workers, assembly line workers, musicians, and athletes are among the most vulnerable groups. The prevalence is higher in women, potentially due to differences in occupational roles and physical structure.
Manual Therapy encompasses a range of hands-on techniques performed by physical therapists or myotherapists to alleviate RSI symptoms. Key techniques include:
- Massage therapy: Targets soft tissues to reduce muscle tension, improve circulation, and promote relaxation.
- Joint mobilisations: Gentle, controlled movements of joints to restore range of motion and alleviate pain.
- Soft tissue mobilisations: Techniques such as myofascial release to break down scar tissue and adhesions in muscles and connective tissues.
- Trigger point therapy: Applying pressure to specific points to relieve muscle knots and referred pain.
- Stretching and Strengthening exercises: Personalised exercises to improve flexibility, strength, and posture, reducing risk of future injury.

Listed below are some details of a client dealing with a shoulder RSI who is seeking treatment here at HBM, which may also serve as a case study:
Age: 35+
Gender: M
Symptoms: Shoulder pain after cricket match
Medical history: MRI showing slight oedema in subacromial bursa
Lifestyle: Sitting for work mainly, but workstation is not set up ergonomically; recently started playing cricket again.
The client has received 4 treatments here at HBM over 3 months to manage his symptoms, and even after the first treatment has had great improvement in mobility and pain. Educating him on the importance of compliance to treatment due to his active schedule has made a big difference on his quality of life, and after educating him on the possible cause (after numerous questioning and orthopaedic testing) and with some take home exercises and stretches, he’s been able to get back to his daily activities with much improvements on symptoms.
If you or someone you know are dealing with RSI, musculoskeletal pain, or even myofascial trigger points, book in an appointment to see us now for an initial consultation so we can assess your condition and come up with an appropriate and tailored treatment plan to manage your pain.
Simply click this booking link for the myotherapy initial consultation with our experienced myotherapists.





 The pathophysiology of CTS is complex and involves mechanical compression, ischemia, and inflammation of the median nerve within the carpal tunnel. Predisposing factors such as wrist anatomy, repetitive hand movements, trauma, hormonal changes, and systemic diseases contribute to the development of CTS. Compression of the median nerve leads to impaired nerve conduction, demyelination, and axonal degeneration, resulting in sensory and motor deficits in the affected hand.
The pathophysiology of CTS is complex and involves mechanical compression, ischemia, and inflammation of the median nerve within the carpal tunnel. Predisposing factors such as wrist anatomy, repetitive hand movements, trauma, hormonal changes, and systemic diseases contribute to the development of CTS. Compression of the median nerve leads to impaired nerve conduction, demyelination, and axonal degeneration, resulting in sensory and motor deficits in the affected hand. If you or someone you know are dealing with CTS, musculoskeletal pain, or even myofascial trigger points, book in an appointment to see us now for an initial consultation so we can assess your condition and come up with an appropriate and tailored treatment plan to manage your pain.
If you or someone you know are dealing with CTS, musculoskeletal pain, or even myofascial trigger points, book in an appointment to see us now for an initial consultation so we can assess your condition and come up with an appropriate and tailored treatment plan to manage your pain.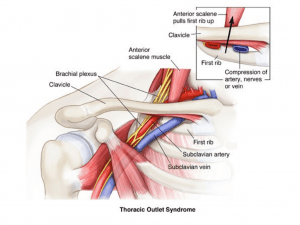

 Individuals with LCS often experience chronic low back pain, hip pain, and tightness in the hip flexors. Dysfunction in the lumbar-pelvic region may contribute to secondary symptoms such as sacroiliac joint dysfunction and hip joint impingement. Additionally, LCS can impair functional movement patterns, affecting activities such as walking, standing, and squatting. Reduced hip mobility and stability may also predispose individuals to compensatory movements and increased risk of injury during physical activities.
Individuals with LCS often experience chronic low back pain, hip pain, and tightness in the hip flexors. Dysfunction in the lumbar-pelvic region may contribute to secondary symptoms such as sacroiliac joint dysfunction and hip joint impingement. Additionally, LCS can impair functional movement patterns, affecting activities such as walking, standing, and squatting. Reduced hip mobility and stability may also predispose individuals to compensatory movements and increased risk of injury during physical activities.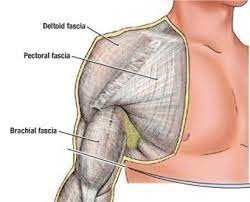 Some of the common fascial conditions include Myofascial Pain Syndrome (MPS), which is a pathology characterised by the development of trigger points within fascial tissues. These trigger points can lead to localised or referred pain, muscle stiffness, and reduced range of motion. Another fascial condition that may arise is fascial adhesions, which occur when collagen fibers in the fascial matrix become distorted or adhered, resulting in restricted movement and impaired tissue glide. This can contribute to chronic pain and dysfunction.
Some of the common fascial conditions include Myofascial Pain Syndrome (MPS), which is a pathology characterised by the development of trigger points within fascial tissues. These trigger points can lead to localised or referred pain, muscle stiffness, and reduced range of motion. Another fascial condition that may arise is fascial adhesions, which occur when collagen fibers in the fascial matrix become distorted or adhered, resulting in restricted movement and impaired tissue glide. This can contribute to chronic pain and dysfunction.









