Relieve Tight Shoulders: A Myotherapist’s Guide to Trapezius Health
Author: Jerry Song
The trapezius muscle is one of the most prominent and multifunctional muscles in the human body. It plays a vital role in movement, posture, and stability, but it’s also prone to tension and pain. Whether due to prolonged desk work, heavy lifting, or stress, the trapezius often develops trigger points, leading to discomfort that can impact daily activities.
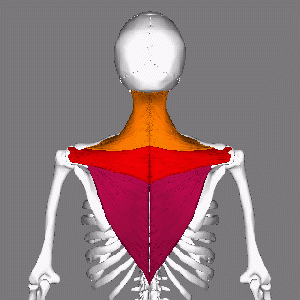
Anatomy of the Trapezius Muscle
The trapezius is a large, flat, diamond-shaped muscle that spans across the upper back and neck. It is divided into three distinct regions:
- Upper trapezius: Originates at the base of the skull and runs down to the shoulders.
- Middle trapezius: Spans from the upper thoracic spine to the shoulder blades.
- Lower trapezius: Extends from the mid-thoracic spine to the lower shoulder blades.
Primary Functions:
- Upper trapezius: Elevates the shoulders (e.g., shrugging) and assists in neck movement.
- Middle trapezius: Retracts the scapula (pulls shoulder blades together).
- Lower trapezius: Depresses and stabilises the scapula.
The trapezius muscle is essential for maintaining good posture, facilitating head and shoulder movement, and stabilising the upper body during physical activity.
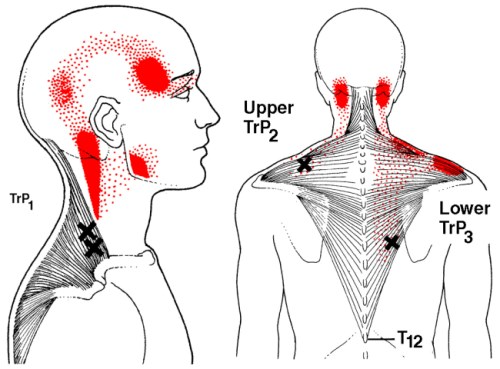
Common Trigger Points in the Trapezius
Trigger points are hyper-irritable knots within the muscle fibers that cause localised pain and may refer discomfort to other areas. The trapezius is one of the most common muscles to develop trigger points.
Typical Trigger Point Locations:
- Upper trapezius: Often found near the base of the skull or at the midpoint between the neck and shoulder.
- Middle trapezius: Near the spine, along the shoulder blades.
- Lower trapezius: Along the lower edge of the shoulder blade and thoracic spine.
Referred Pain Patterns:
- Pain may radiate to the neck, head (often mistaken for tension headaches), shoulders, or upper back.
- Upper trapezius trigger points frequently cause pain at the base of the skull or in the temples, mimicking a migraine.
Certain demographics and activities make individuals more prone to trapezius trigger points:
- Office Workers and Students
- Long hours of sitting with poor posture or forward head position.
- Stress and tension, leading to elevated shoulders and clenched muscles.
- Athletes
- Sports involving repetitive shoulder movements, such as swimming, tennis, or weightlifting, can overwork the trapezius.
- Manual Labourers
- Lifting heavy objects or prolonged physical strain can cause overuse of the trapezius.
- Chronic Stress Sufferers
- Emotional stress often manifests physically, with the trapezius holding tension as a protective response.
- Older Adults
- Age-related changes, like reduced muscle elasticity and weakened posture, increase susceptibility.

Myotherapy offers a range of techniques to address trapezius dysfunction, reduce trigger points, and restore proper muscle function. Commonly used treatments include:
- Trigger Point Therapy
- Direct pressure is applied to trigger points to deactivate them and relieve pain.
- Dry Needling
- Thin needles are inserted into trigger points to release muscle tension and improve circulation, reducing pain and promoting healing.
- Myofascial Release
- Gentle, sustained pressure is used to stretch the fascia (connective tissue) around the trapezius, reducing tightness and restoring mobility.
- Massage Therapy
- Techniques like effleurage, petrissage, and deep tissue massage help relax the muscle, reduce inflammation, and improve blood flow.
- Stretching and Mobility Exercises
- Myotherapists provide tailored stretches to lengthen the trapezius and improve its flexibility.
- Example: Neck tilts or shoulder shrugs can help relieve tightness in the upper trapezius.
- Postural Assessment and Correction
- A myotherapist evaluates posture to identify contributing factors, such as forward head posture or rounded shoulders, and recommends ergonomic adjustments.
- Heat and Cold Therapy
- Heat application increases blood flow and relaxes the muscle, while cold therapy reduces inflammation and acute pain.
- Strengthening Exercises
- Weakness in the trapezius can cause overcompensation by other muscles, leading to tension. Strengthening the lower and middle trapezius can help rebalance the area.

Tips for Preventing Trapezius Tension
Incorporating the following habits into your daily routine can reduce the risk of developing trapezius-related issues:
- Practice Good Posture: Keep your shoulders relaxed, neck neutral, and head aligned with your spine.
- Take Frequent Breaks: If you work at a desk, stand up and stretch every 30-60 minutes.
- Manage Stress: Regular relaxation techniques, such as deep breathing or meditation, can prevent tension buildup.
- Stay Active: Engage in exercises that strengthen your back, shoulders, and core to support your posture.
-
Stretch Regularly: Incorporate neck and shoulder stretches into your routine to maintain flexibility.
The trapezius muscle plays a crucial role in maintaining posture, facilitating movement, and supporting overall upper-body function. However, it’s also highly prone to tension and trigger points, especially in today’s sedentary, high-stress lifestyles. While we’ve focused on the trapezius in this article, it’s important to note that in most cases, pain arises from multiple contributing factors, including other muscles, joints, and overall movement patterns. For this reason, it’s always best to seek a proper assessment from an experienced therapist to identify the root cause of the issue and develop an effective treatment and self-care plan.
If you or someone you know are dealing with a trapezius condition, musculoskeletal pain, or even myofascial trigger points, book an appointment to see Jerry now for an initial consultation so we can assess your condition and come up with an appropriate and tailored treatment plan to manage your pain. Simply click this booking link for the myotherapy initial consultation with our experienced myotherapists.
 .
. 







