The Overlooked Facts of Fascia
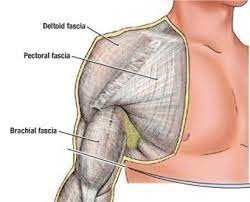
Fascia is a complex, three-dimensional network of connective tissue that pervades the entire human body, surrounding and interpenetrating muscles, bones, nerves, and organs. Fascia consists of collagen fibers, elastin, ground substance, and cells such as fibroblasts. The arrangement of these components contributes to the diverse mechanical properties of fascial tissues. Fascia serves as a dynamic system with several key functions, including providing structural support, facilitating movement and flexibility, and participating in proprioception. Moreover, it acts as a conduit for neurovascular structures and plays a vital role in intercellular communication.
 Some of the common fascial conditions include Myofascial Pain Syndrome (MPS), which is a pathology characterised by the development of trigger points within fascial tissues. These trigger points can lead to localised or referred pain, muscle stiffness, and reduced range of motion. Another fascial condition that may arise is fascial adhesions, which occur when collagen fibers in the fascial matrix become distorted or adhered, resulting in restricted movement and impaired tissue glide. This can contribute to chronic pain and dysfunction.
Some of the common fascial conditions include Myofascial Pain Syndrome (MPS), which is a pathology characterised by the development of trigger points within fascial tissues. These trigger points can lead to localised or referred pain, muscle stiffness, and reduced range of motion. Another fascial condition that may arise is fascial adhesions, which occur when collagen fibers in the fascial matrix become distorted or adhered, resulting in restricted movement and impaired tissue glide. This can contribute to chronic pain and dysfunction.
The Role of Manual Therapy in Fascial Treatment:
- Soft Tissue Mobilisation:
Manual therapy techniques, such as soft tissue mobilisation, aim to address fascial restrictions by applying controlled pressure and movement to specific areas. This helps to break down adhesions, improve tissue flexibility, and restore normal function.
- Myofascial Release:
Myofascial release involves sustained pressure and stretching of fascial tissues to release tension and promote optimal tissue mobility. Therapists use various hands-on techniques to target specific areas of fascial restriction.
- Instrument-Assisted Soft Tissue Mobilisation (IASTM):
IASTM employs specialised tools to detect and treat fascial dysfunction. By applying controlled pressure through these instruments, therapists can break down adhesions and enhance the healing response.

Aside from the above, myofascial cupping and dry needling are two therapeutic modalities that can be effective in addressing fascial conditions, contributing to improved tissue mobility, pain relief, and overall well-being.


Cupping involves placing suction cups on the skin, creating a negative pressure environment. This negative pressure lifts the fascial layers, increasing blood flow and promoting the release of fascial restrictions. The suction effect can also create a separation between the layers of fascia, reducing adhesions and facilitating better tissue glide. Cupping is believed to also stimulate the lymphatic system, aiding in the removal of toxins and metabolic waste from the fascial tissues.
Dry needling involves the insertion of thin, solid needles into trigger points or tight bands of fascial tissue. These trigger points are areas of hyperirritability within the fascia. The needling creates a microtrauma, prompting a local twitch response in the muscle fibers. This response helps release tension and reset the neuromuscular system.
Listed below are some details of a client dealing with lower back pain who is seeking treatment here at HBM, which may also serve as a case study:
Age: 40+
Gender: M
Symptoms: Sensation of tightness in the lower back and forearms
Medical history: Disc bulge injury in L4-S1 in the past, Tennis elbow
Lifestyle: Works at a desk and sits in front of a screen for long periods. Did a lot of boxing until recently, when he increased his weightlifting sessions.
The client has received 3x treatments here at HBM over 1.5 months to manage his symptoms, and even after the first treatment has had great improvement in mobility. Educating him on the importance of compliance to treatment has made a big difference on his quality of life.
If you or someone you know are dealing with lower back pain, tennis elbow, headaches/migraines, and think it may be due to a fascial condition, book in an appointment to see us now for an initial consultation so we can assess your condition and come up with an appropriate and tailored treatment plan to manage your pain.
Simply click this booking link for the myotherapy initial consultation with our experienced therapists.