Common Conditions Addressed by Cupping Therapy
Author: Holly Xu
Cupping therapy, an ancient healing practice with roots in traditional Chinese medicine and Middle Eastern cultures, has gained significant popularity in modern wellness for its wide-ranging health benefits. By creating suction on the skin, cupping stimulates blood flow,
releases tension, and promotes the body’s natural healing processes. Below, we explore some of the common conditions that can be addressed through this therapeutic modality, alongside patient case examples.

- Muscle Tension and Pain
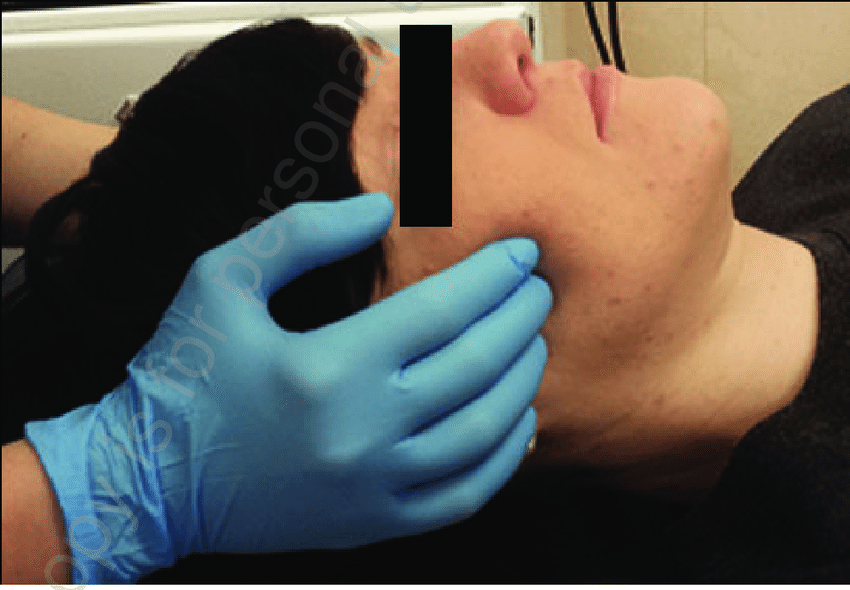
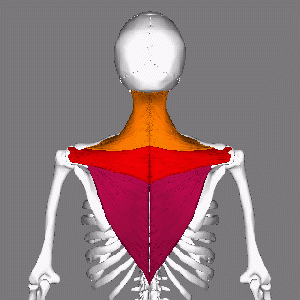
Cupping therapy is highly effective in alleviating muscle tension and pain, making it a popular choice for athletes and individuals with physically demanding lifestyles. The suction created by the cups helps increase blood circulation to the affected areas, reducing stiffness and promoting faster recovery.
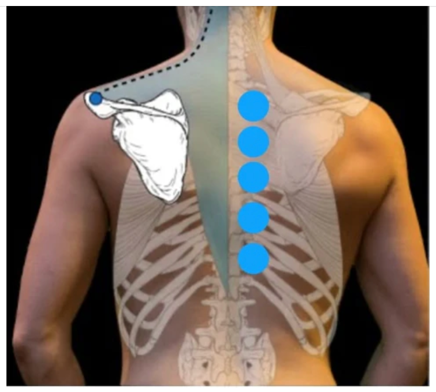
Case Example: Jane, a 35-year-old office worker, suffered from chronic neck and shoulder tension due to long hours at her desk and not so ergonomic set up. After a few sessions of cupping therapy focusing on her upper back and shoulders, she experienced a significant reduction in pain and improved range of motion, allowing her to work more comfortably. She happily left a five stars Google review after the treatment plan of six sessions,
——–“I go to Holly and she is like magic. I’ve had neck and shoulder pains and she has helped me fix my issues and also skin issues through cupping. I’m so glad I came across her as she’s helped me a lot with my posture” J.L.
Common conditions include:
- Back and neck pain
- Shoulder tension
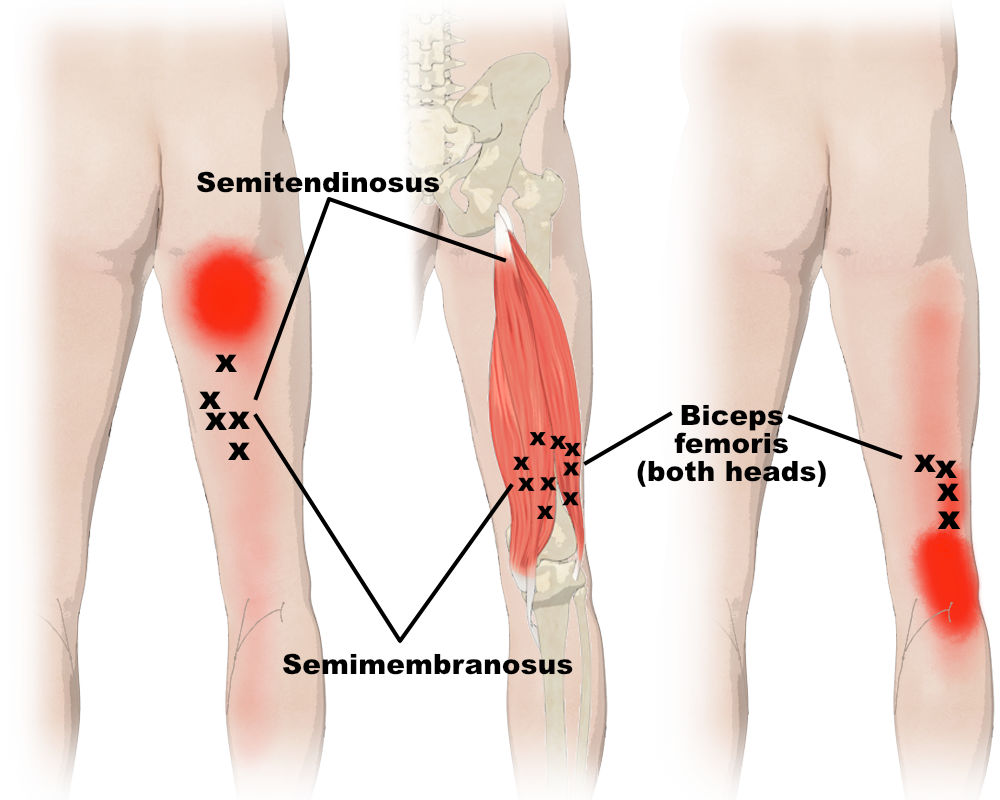
- Tight hamstrings or calves
- General muscle soreness after workouts
- Plantar fasciitis
- Tennis elbow (lateral epicondylitis)
- Golfer’s elbow (medial epicondylitis)
- Rotator cuff strain or tendinitis
- IT band syndrome
- Quadriceps or hip flexor strain
- Chronic Pain Conditions
For individuals suffering from chronic pain conditions, cupping can provide significant relief. Its ability to reduce inflammation and improve circulation makes it a valuable tool in managing:
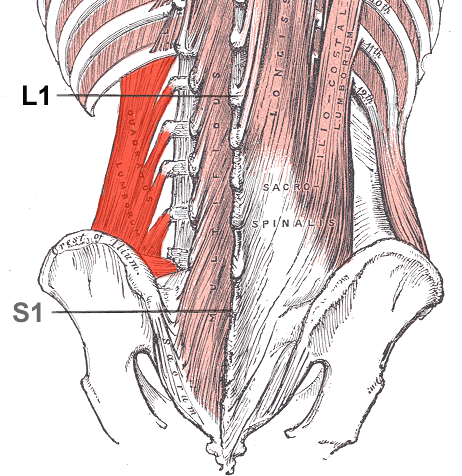
Case Example: Mark, a 50-year-old construction worker, struggled with sciatica that radiated down his leg. Cupping therapy, combined with stretching, targeted his lower back gluteus, and hamstring area, leading to reduced nerve pain and greater mobility.
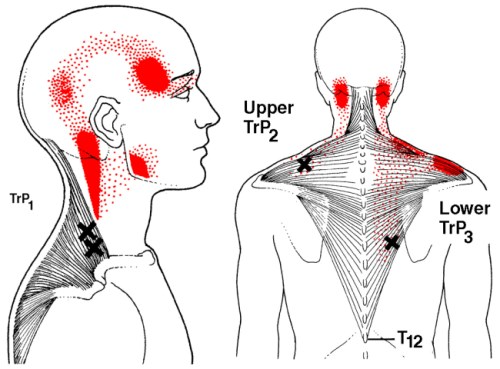
3. Stress and Anxiety
The relaxing effects of cupping therapy extend beyond the physical realm. By calming the nervous system and reducing muscle tension, cupping can help manage stress and anxiety. The therapy’s rhythmic application often promotes a meditative state, allowing clients to unwind and reset.
Case Example: Emma, a 29-year-old teacher, found herself overwhelmed by stress and tension headaches. Regular cupping sessions targeting her upper back and neck helped her relax and significantly reduced the frequency of her headaches.
- Respiratory Issues
Cupping has long been used to address respiratory conditions by loosening congestion and improving lung function. It can be beneficial for:
- Asthma
- Bronchitis
- Chronic cough
- Sinus congestion
- Digestive Health
Cupping therapy can also support digestive health by stimulating the abdominal area, promoting better blood flow to the digestive organs, and reducing tension in the gut. It may be used to help alleviate:
- Irritable Bowel Syndrome (IBS)
- Bloating
- Constipation
- Stomach cramps
- Postural Imbalances
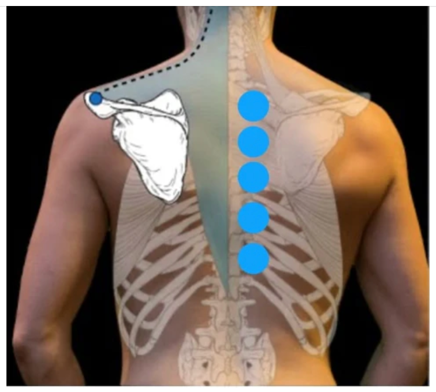
Many people experience postural imbalances due to prolonged sitting, poor ergonomics, or repetitive movements. Cupping therapy can help realign the body by relieving tension in overworked muscles and promoting better mobility.
Case Example: Alex, a 30-year-old graphic designer, noticed chronic lower back pain due to poor posture. After undergoing a series of cupping treatments, paired with ergonomic adjustments, his posture improved, and his pain decreased.
Alex left below Google review,
“Holly has helped transform my body and all of my aches and pains have gone away. My flexibility has improved and my back pain is no longer a burden. 10/10 recommend.”
- Scar Tissue and Adhesions
The suction from cupping can soften and break down scar tissue, reducing restrictions caused by old injuries or surgeries. This allows for improved mobility and reduced discomfort in the affected areas.
- Improved Skin Health
Cupping therapy is also beneficial for skin conditions such as acne, eczema, and even cellulite. The increased blood flow to the surface of the skin promotes healing, reduces inflammation, and enhances the skin’s overall appearance.

Is Cupping Therapy Right for You?

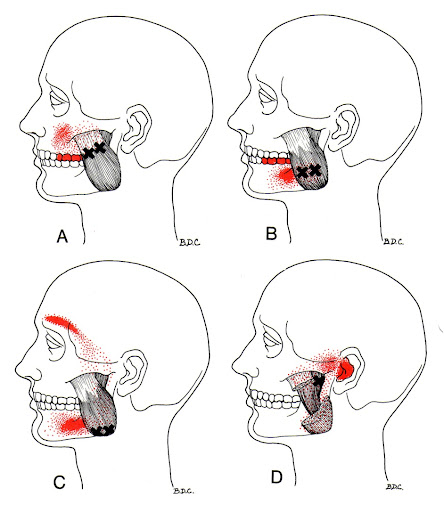
While cupping therapy offers numerous benefits, it is important to consult with a qualified practitioner to ensure it is suitable for your specific condition. At Holistic Balance Myotherapy, we provide tailored treatment plans that incorporate cupping therapy alongside other modalities such as Trigger point therapy, Dry needling etc to address your unique needs. Whether you’re seeking relief from chronic pain or simply looking to enhance your overall well-being, cupping therapy can be a valuable addition to your self-care routine.
Please Book your initial myotherapy consultation with our experienced myotherapists to explore how cupping therapy can support your health journey.